Irritable bowel syndrome (IBS) can be a frustrating foe. It disrupts your day with abdominal pain, throws your bowel habits into disarray, and often leaves you feeling like there’s nowhere to turn. But fear not, there’s much to understand about IBS, and with the right knowledge, you can manage it effectively.
Contents
What is IBS?
Imagine your digestive system as a complex orchestra. In IBS, the instruments – your intestines, muscles, and nerves – aren’t necessarily damaged, but they’re not playing in perfect harmony. This creates a symphony of discomfort, with cramping, bloating, and irregular bowel movements taking center stage.
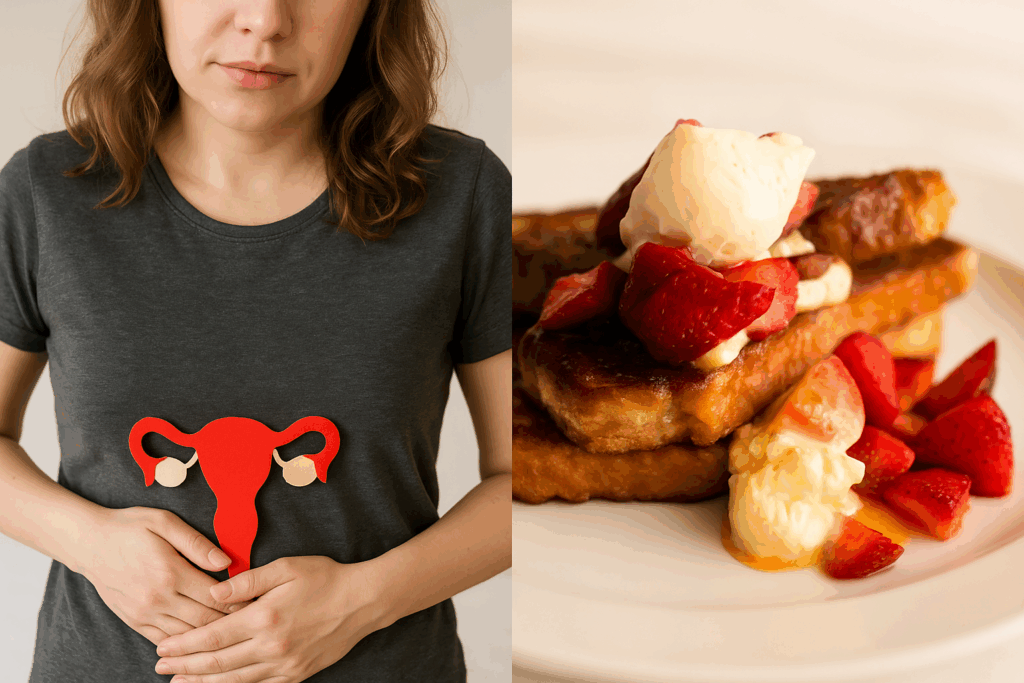
IBS is classified as a functional gastrointestinal (GI) disorder. This means there’s no visible damage to the digestive tract, but the communication between your gut and brain gets a little scrambled. Stress, certain foods, and even hormones can disrupt this delicate dance, leading to IBS flare-ups.
The Three Faces of IBS
While the core symptoms of IBS are abdominal pain and altered bowel movements, the way these manifest can vary. Doctors categorize IBS into three main types based on the predominant bowel issues:
IBS with constipation (IBS-C): This type is characterized by infrequent bowel movements (less than three per week) and hard, lumpy stools.
IBS with diarrhea (IBS-D): Here, the opposite occurs. You experience frequent bowel movements (more than three per day) with loose, watery stools.
IBS mixed (IBS-M): This is the most common type, where you experience a combination of constipation and diarrhea.
IBS and its Unwanted Guests
IBS often comes with unwelcome companions. You might experience other health conditions alongside it, such as:
- Fibromyalgia: Chronic pain throughout the body, especially in muscles and joints.
- Chronic fatigue syndrome: Extreme tiredness that doesn’t improve with rest.
- Chronic pelvic pain: Long-lasting pain in the lower abdomen or pelvic area.
- Dyspepsia: Indigestion and discomfort in the upper part of the abdomen.
- Gastroesophageal reflux disease (GERD): Heartburn and regurgitation of stomach contents.
- Anxiety and depression: Mental health conditions that can worsen IBS symptoms and vice versa.
- Somatic symptom disorder: Physical symptoms that can’t be explained by a medical condition.
The Road to Relief: Managing IBS
Though there’s no cure for IBS, the good news is you can effectively manage it and significantly improve your quality of life. Here are some key strategies:
- Diet: Identify food triggers that worsen your symptoms. Consider a low FODMAP diet, which helps manage certain poorly absorbed carbohydrates.
- Stress Management: Stress can be a major trigger for IBS flare-ups. Techniques like yoga, meditation, and deep breathing can help.
- Fiber: Adequate fiber intake can regulate bowel movements and ease constipation.
- Medication: Antidiarrheal medications, laxatives, and medications to manage pain and cramping can be helpful.
- Talk Therapy: Cognitive behavioral therapy can help you develop coping mechanisms to deal with stress and improve your relationship with IBS.
Remember, you’re not alone! IBS is a prevalent condition, and there’s a wealth of resources available. Talk to your doctor, explore online support groups, and educate yourself. By taking an active role in managing your IBS, you can reclaim control of your well-being and live a comfortable, fulfilling life.


 Call Us
Call Us
 Locate Us
Locate Us